Can Vegetarian Diet Help Ulcerative Colitis
Make simple, consistent improvements to your diet and nutrition to better manage your colitis symptoms. A nutritionist for Colitis can be the perfect partner to your primary care doctor to help you manage your Ulcerative Colitis. Our evidence-based process can help you implement proven strategies to feel better and improve your health. Currently Reading Chapter Name Appears Here Although there is no "cure" for Ulcerative Colitis, combining traditional medicine with the recommendations from our Registered Dietitians can help you re-establish a normal routine and feel healthier. Our Registered Dietitians help you determine: Colitis, Ulcerative Colitis, and Crohn's are often used interchangeably - but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining (colon). It is synonymous with Irritable Bowel Disease (IBD) and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine. Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn's Disease here. What if Affects Ulcerative Colitis specifically affects your large intestine, also known as the large bowel or colon. The ulcers form on only the top layer of tissue in your colon Anywhere along your GI tract, although it is commonly found in the small intestine and large intestine. Crohn's impacts all tissue layers at its site Crohn's can also cause issues with your skin, eyes, and joints Symptoms Treatment Diagnosis: performed by a gastroenterologist Our summary of the two conditions is below. You can also read a more detailed explanation about thedifferences between Colitis and Crohn's Disease here. Take your reading on the go and download the PDF, included with your downloadable guide is a 7-day meal plan complete with easy-to-follow recipes. If you have Ulcerative Colitis, very minor changes to what you eat can make a BIG difference in your symptoms. Consider keeping food logs or adjusting foods that trigger your symptoms. You may also want to work with your doctor or dietitian to work through an elimination diet. Generally, you should try to: In terms of specific food recommendations, go with these: Lean Protein Low Fiber Fruits Veggies Veggies can be hit or miss, so be be very specific: Foods with Probiotics During a flare up, you many find it more comfortable to eat bland, soft food, otherwise limiting spicy foods. During periods of remission, you should eat all of your usual items with the omission of known offenders. Most importantly, we highlight that each person's food sensitivities and triggers are different Below is a list ofcommontrigger foods; keep in mind that they vary for each person We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently You may find a "Low Residue" approach helpful. We have seen it work well for some people Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day Some studies show that a higher fiber diet can improve IBD conditions Go beyond what you're learning in this guide, included with the downloadable PDF is a 7-day meal plan complete with easy-to-follow recipes. A dietitian with an expertise in GI and digestive issues, such as OnPoint! Always consult your primary care doctor. They can refer you to a local GI specialist if needed If diagnosed, you may want to seek a specialist for your specific disease in your area According to George Washington University, colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease (IBD) and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon. The following diseases fall into the colitis/IBD category; they all can be treated with a combination of medication and improvements to your eating habits: Ulcerative colitis is a chronic inflammatory bowel disease (IBD) in which abnormal reactions of the immune system cause inflammation and ulcers on the inner lining of your large intestine. Ulcerative colitis can develop at any age, but the disease is more likely to develop in people between the ages of 15 and 30. Read more below! Crohn's disease is an inflammatory bowel disease that causes chronic inflammation of the gastrointestinal tract. Recent research suggests hereditary, genetic, and environmental factors contribute to Crohn's disease development. In people with Crohn's, harmless bacteria are mistaken for foreign invaders and the immune system mounts a response. The inflammation caused by the immune response does not go away. This leads to chronic inflammation, ulceration, and thickening of the intestinal wall. Diversion colitis involves inflammation in the large intestine brought on after surgical treatment that diverts the fecal stream away from the large intestine, usually to a temporary ileostomy or colostomy. It should not be confused with being a type of inflammatory bowel disease (IBD), even though it often mimics the symptoms of IBD. Diversion colitis can occur after surgical treatment for intestinal-related conditions such as fecal incontinence, bowel cancer, or spontaneous chronic constipation that is not related to an obvious underlying cause. Ischemic colitis (IC) is an inflammatory condition of the large intestine, or colon. It develops when there isn't enough blood flow to the colon. IC can occur at any age, but it's most common among those over the age of 60.A buildup of plaque inside the arteries (atherosclerosis) can cause chronic, or long-term, IC. This condition may also go away with mild treatment, such as a short-term liquid diet and antibiotics. Colonic infection by bacteria, viruses, or parasites results in an inflammatory-type of diarrhea and accounts for the majority of cases presenting with acute diarrhea. These patients present with purulent, bloody, and mucoid loose bowel motions, fever, tenesmus, and abdominal pain. Fulminant colitis is a somewhat rare but serious form of ulcerative colitis (UC). UC causes inflammation and sores in the lining of the colon. It doesn't happen to most people who have UC. Less than 10% of people with it get fulminant colitis, usually during their first attack of symptoms. The whole lining of the colon becomes inflamed, causing severe symptoms like bloody diarrhea and belly pain. Fulminant colitis is a medical emergency. You'll need to go to a hospital right away for treatment with medicine, and possibly surgery. Collagenous colitis (CC) is a condition that affects your large intestine. It leads to episodes of watery diarrhea and belly pain. Your large intestine is part of your digestive (gastrointestinal or GI) tract. The GI tract goes from your mouth all the way to your rectal opening. The large intestine includes both the colon and the rectum. The large intestine receives the broken-down products of food from the small intestine. One of its main jobs is to reabsorb water and electrolytes, such as salt. The colon leads to the rectum. The rectum stores your bowel movements before your body eliminates them. In Collagenous colitis, inflammatory cells from your immune system travel to your large intestine. There they cause swelling and inflammation. In rare cases, these cells also go into the latter part of your small intestine. Chemical colitis is a type of colitis, an inflammation of the large intestine or colon, caused by the introduction of harsh chemicals to the colon by an enema or other procedure. Chemical colitis can resemble ulcerative colitis, infectious colitis and pseudomembranous colitis endoscopically. Microscopic colitis is an inflammation of the large intestine (colon) that causes persistent watery diarrhea. The disorder gets its name from the fact that it's necessary to examine colon tissue under a microscope to identify it, since the tissue may appear normal with a colonoscopy or flexible sigmoidoscopy. There are different subtypes of microscopic colitis: Collagenous colitis, in which a thick layer of protein (collagen) develops in colon tissue; Lymphocytic colitis, in which white blood cells (lymphocytes) increase in colon tissue; Incomplete microscopic colitis, in which there are mixed features of collagenous and lymphocytic colitis. In lymphocytic colitis, inflammatory cells from your immune system travel to your large intestine. Here they cause swelling and inflammation of the tissues. In rare cases, these cells also invade the latter part of the small intestine. Immune cells (lymphocytes) may build up in the area as well. The inflammation may keep your large intestine from reabsorbing as much water as it should. This leads to diarrhea, belly pain, and other symptoms. Your symptoms are unique to you. Your nutritionist tracks your food with you and makes specific recommendations to help you feel better. Based upon your daily routine, we will build a custom plan to help alleviate your GI and IBD issues. Success does not happen overnight. If something isn't working quite right, we make changes right away.Ulcerative Colitis Diet

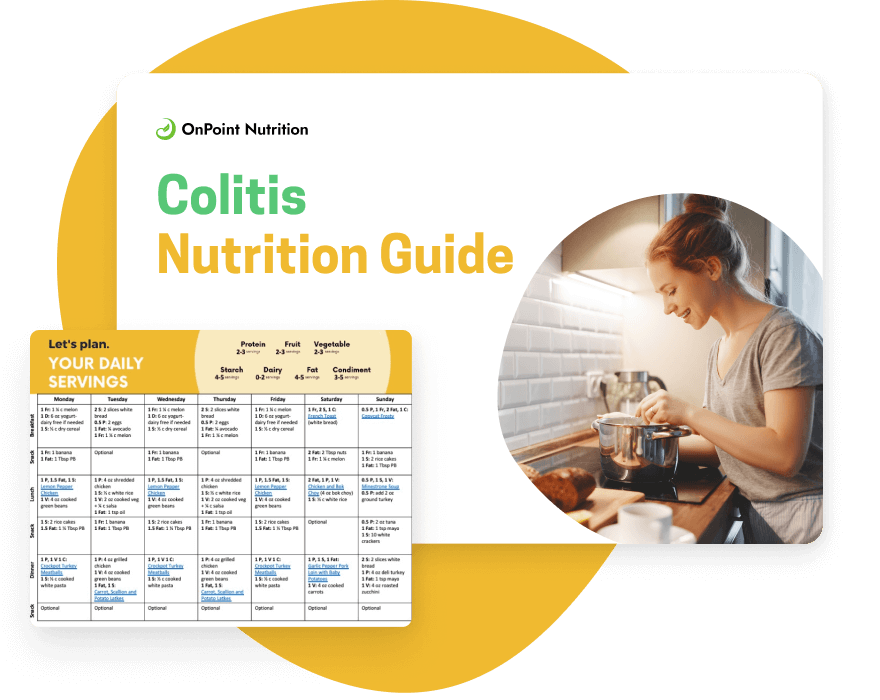
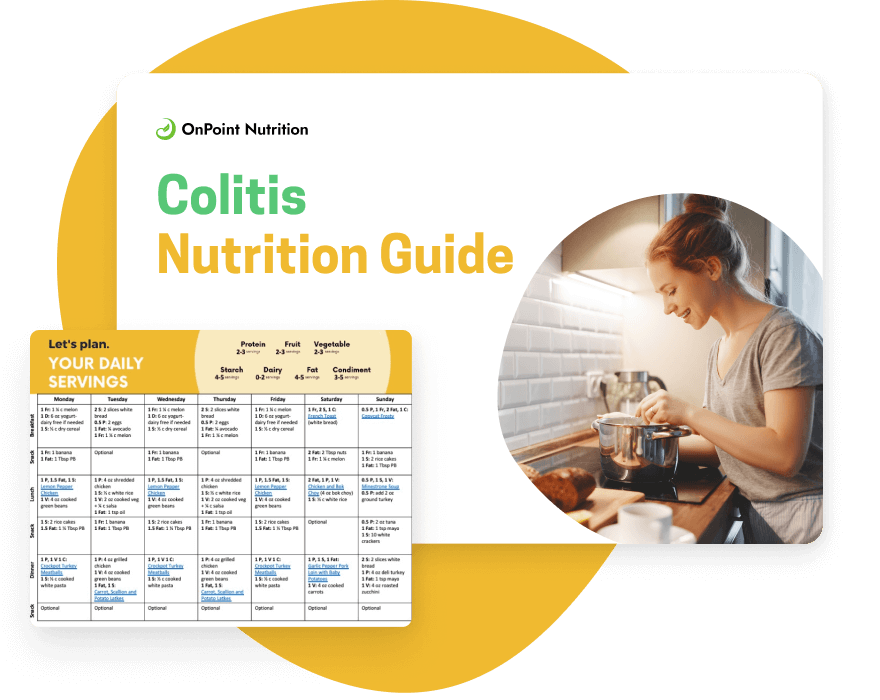
Build a tailored nutrition plan to treat your colitis
Alleviate your Ulcerative Colitis symptoms with a meal plan customized to your individual needs.
Ulcerative Colitis: Let's Talk
Ulcerative Colitis: this is why you're here, right?
It can be challenging to differentiate between Crohn's and UC
Ulcerative Colitis Crohn's Disease
Improve your Ulcerative Colitis symptoms and take action — today!

What foods should you eat with Ulcerative Colitis?
Food Type Examples
And for plant-based diets:
Foods to avoid with Ulcerative Colitis
I have heard that fiber is good for Ulcerative Colitis. What does OnPoint Say?
Reduce flare-ups, gain energy, and improve your quality of life.

Who to contact if you have questions about Ulcerative Colitis
More information about Ulcerative Colitis
Ulcerative colitis:
Crohn's colitis:
Diversion colitis:
Ischemic colitis:
Infectious colitis:
Fulminant colitis:
Collagenous colitis:
Chemical colitis:
Microscopic colitis:
Lymphocytic colitis:
Our Team Listens
A plan built just for you
Continuous Improvement
Our dietitians and nutritionists build custom plans tailored to help you find relief from your GI issues. Our expertise includes: IBS, Crohn's Disease, and Ulcerative colitis We would love to meet you!
Submit your question directly to our team
"We have worked with hundreds of clients who live with GI issues such as Ulcerative Colitis. We know how hard it can be to live with the condition. We hope you will allow us to help you tackle your GI issue head-on."

Can Vegetarian Diet Help Ulcerative Colitis
Source: https://www.onpoint-nutrition.com/colitis-diet
0 Response to "Can Vegetarian Diet Help Ulcerative Colitis"
Post a Comment